Over the past year, the Centers for Medicare & Medicaid Services (CMS) has been signaling the continued evolution of value-based care for the future. In early 2019, we saw an overhaul of the Medicare Shared Savings Program (MSSP) as CMS rolled out the new Pathways to Success program. The new model continues to move organizations down paths to higher risk arrangements. Initially, the MSSP market responded with general uncertainty at the prospect of enhanced risk. We saw large groups begin to question their ability to succeed in the future, and there was a temporary stall in the number of new ACOs. Still, CMS has remained steadfast in their views that organizations must solidify a secure value-based care strategy and use early programs to adopt and test best practices in their specific market contexts.
As we are a quarter of the way through 2020, the industry has continued to signal that organizations will need to understand and adapt to value-based care arrangements. With the introduction of the Primary Care First (PCF) and Direct Contracting (DC) models, organizations must develop a clear understanding of population segmentation, HCC coding, high-risk patient management, and post-acute care collaboration. Each of these programs has elements of a full-risk Medicare Advantage arrangement and are providing stepping stones for organizations to test and incubate their long term value-based care strategy.
CMS has also expanded chronic care management (CCM) and remote patient monitoring programs to reduce the administrative burden on practices and allow them to better capitalize on their value-based care programs. These steps indicate a recognition that the programs require practice transformation and that physician leaders are going to have to reorganize how they staff and run their practices. Almost as an olive branch, CMS announced measures to reduce physician coding and administration. These are both positive signs that CMS is removing barriers in these arrangements. As CMS continues to signal the market, payers and MCOs are starting to align many of their agreements to mirror these changes.
Although change often causes uncertainty in organizations, Lightbeam is confident that there will be a continual push toward downside risk arrangements. We have continued to monitor the population health space and design methods that enable practices to succeed in ever-changing programs. Our best in class end-to-end solutions are well suited for early-stage adoption or full-risk capitated arrangements. It is essential to begin using the tools that CMS is offering to understand better how to bridge fee-for-service to value-based payments, reorganize and shift resources at the clinic level, redistribute physician compensation models, and select quality and cost-effective referral network partners.
Turning Uncertainty into Certainty
There are several critical steps to understand your current value-based maturity level and readiness. Below is our Organizational Maturity Model:
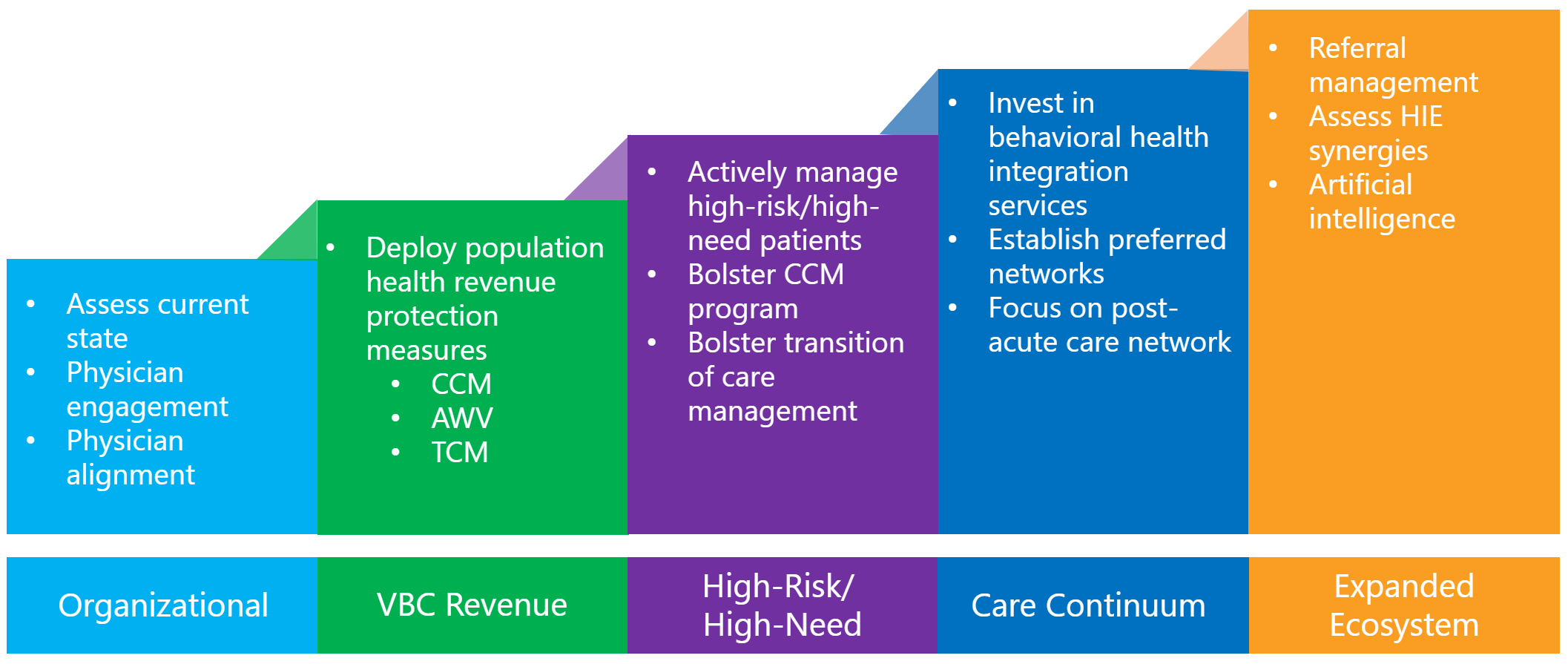
At the heart of your organizational assessment, you should be able to identify your percentage of value-based contracts as a total book of business. Our advisory services team can then help review contracts and determine the right initiatives to focus on to move your organization to the next tier. Our goal is to bring clarity and strategy in a few of the following areas that CMS has continued to signal as important factors for population health. Below are questions that you will need to have a firm understanding of to be successful in the evolving models.
Practice Transformation
- Do you have a clear physician compensation strategy that aligns with a shift from FFS to VBC?
- Do you have a strategy to engage both primary care and specialists in the work of value-based care?
- Do you have a simple strategy to identify and communicate priorities to your physicians?
- Have you staffed the appropriate ratio of mid-levels to build support around your physician and capitalize on revenue-generating programs (CCM, TCM, AWV)?
Population Health Management
- What is your strategy to identify and segment your patient population for care management, disease management, complex management, and proactive wellness?
- Will you deploy a centralized team to help with CCM or TCM programs or staff at the clinic levels only?
- What support structure do you have in place to help your physicians with palliative care, behavioral health issues, community resource needs, and social determinants of health?
Network and Preferred Partner Management
- Do you have a system to accurately monitor and assess the highest quality and cost-effective providers and facilities across your broader network?
- Once your preferred network is established, do you have a method or tool to help steerage to appropriate providers?
- Do you have integrated relationships and business review meetings with your post-acute care partners: SNF, HHA, LTAC?
Expanded Ecosystem Capabilities
- Is your organization positioned to utilize tools like artificial intelligence to augment and expand the work of your physician staff?
- Do you have a clearly defined interface ecosystem strategy to pull data from Clinical, Claims, HIEs and utilize them to the full capacity to identify opportunities better and proactively deliver care?
All of the above questions should paint a picture that changes are necessary to forge a path in the evolving healthcare ecosystem. My guess is that you are on the right track with many of these, but you will need to continue to push your organization to remain innovative and disciplined in the deployment of future strategies. Lightbeam can be a guide our combination of a best-in-class analytics platform with a wide array of subject matter experts in the above domains. Our mission is to provide the tools you need to feel confident in the world of uncertainty; let us know how we can help.

Josh Patten is the Vice President of Operations.
