At the beginning of December, I hosted a webinar presentation discussing the significant changes that will affect Medicare Advantage (MA) reimbursement in 2021. The most significant difference in MA reimbursement, which has many organizations scrambling, is the 2021 Consumer Assessment of Healthcare Providers and Systems (CAHPS®) measures. CAHPS is a survey conducted annually by accredited vendors and consists of patient experience questions sent to members to complete, collect, and report the outcomes. These measures focus on the patient’s perception of their health plan and their providers. The changes will affect the 2023 Star Ratings; these new measure weights mean CAHPS will make up over 30% of the overall Star Rating— four times more than it once was. In this two-part blog series, I continue the webinar conversation by offering additional insights into MA changes and further guidance on succeeding in this enhanced customer service environment.
Important Updates in the Era of COVID
The COVID-19 pandemic has had significant effects on quality measurement programs this year. The Centers for Medicare & Medicaid Services (CMS) has announced MA plans are not required to submit 2020 HEDIS data covering the 2019 reporting year. Additionally, plans will not need to submit CAHPS survey data for 2020. Instead, health plans can use any HEDIS or CAHPS data they have collected from their quality programs, and HEDIS and CAHPS scores based on the 2018 measure year will be used for the 2021 Star Ratings. For 2022, plans are expected to submit HEDIS data in June 2021, and CAHPS will resume as normal. Cut points, or the points where an MA plan qualifies for its Star Ratings based on outcomes, will not be subject to the 5%-point cap in 2022. However, CMS has adopted the Tukey outlier method of removing outliers before assessing cut points and recognizes the potential for an overall decline in industry performance due to the public health emergency, especially for one to three-star plans.
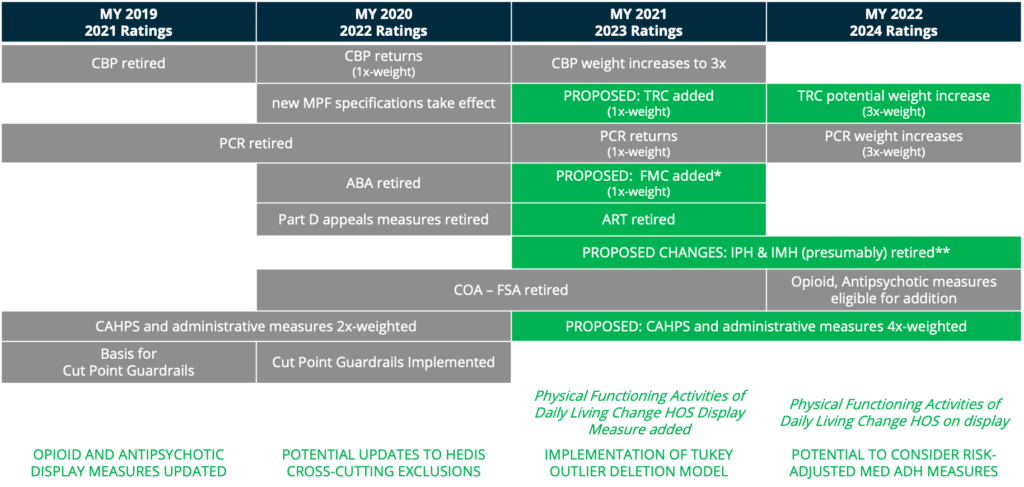
Fig. 1 showcased new, retired, and proposed measures as of February 2020 from “Big Changes Coming to Star Ratings in CMS’ Part 2 Advance Notice & Proposed Rule.” The Gorman Health Group, https://www.gormanhealthgroup.com/blog/star-ratings-changes-cms-advance-notice-proposed-rule/. Accessed December 2020.
The Purpose of the Shift
The overarching question is this: what will these changes mean for healthcare organizations? In short, the 2021 CAHPS changes are intended to stretch MA plans. MA organizations that are comfortable with routine HEDIS measures like mammograms and eye exams must pivot their focus to the patient experience. The score’s breakdown requires that CAHPS becomes a significant priority in keeping ratings viable; CMS anticipates the shift will save the Quality Bonus Program over $4.4 billion in the next ten years.
Organizations that have struggled with CAHPS will need to review their current operations to adapt successfully. It is common for plans to have difficulty moving the needle on the overall patient experience, and they will require focus to monitor patient perception. MA plans who already have implemented member-patient experience teams are likely to continue finding success with CAHPS and possibly grow their Ratings. Next time, I will discuss success strategies to confront these changes to Medicare Advantage in 2021 and other ways to deliver optimal customer service strategies.
To watch my latest webinar on this topic, visit the Lightbeam Education Center.

Cindy Dyer is a Product Manager at Lightbeam.
