A new report from healthcare analytics consulting firm, Avalere Health, indicates lower risk scores in 2021 from the impact of COVID-19. Funded by the Better Medicare Alliance, Avalere based its analysis on Medicare Advantage claims data from 324 million beneficiaries. This consequence will be one of many due to the pandemic, and the lower utilization of healthcare services throughout the year will have adverse effects on patients’ health. Value-based care providers will see a significant drop in risk scores across their populations if they only aggregate claims data and can expect a long journey of catching up next year. With fewer data to base risk scores on, providers will lack the full picture of a patient’s disease status. Consequently, the 2021 MA payments will lower too, and to confront these future challenges, providers will have to go back to the basics to stratify risk and close care gaps.
Findings
The below data table on the 2020 number of MA enrollees this year compared to last was collected for service dates between January 2019 through June 2020. With at least one claim during the analysis period, beneficiaries with at least one claim were down 47% when comparing April 2020 to April 2019, with the public health emergency (PHE) announced in March 2020. The total number of claims decreased by 66% within the same analysis period.
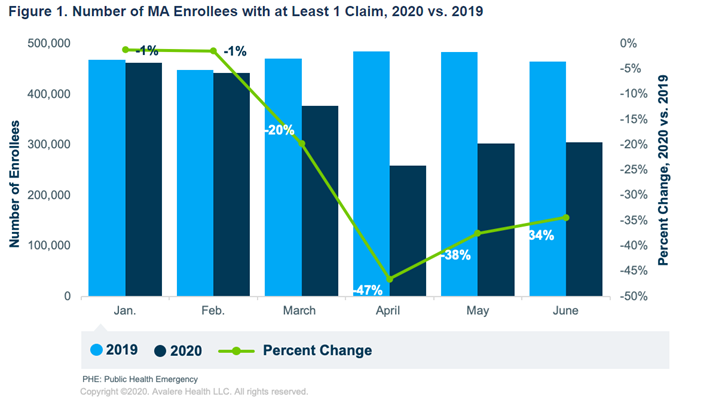
Fig. 1 displays the number of MA enrollees with at least one claim in 2020 versus 2019. From “COVID-19 Pandemic May Reduce MA Risk Scores and Payments.”
The lower utilization decreased providers’ opportunity to code diagnoses, directly impacting 2021 risk adjustment payments for MA plans. Although the health status of enrollees has not changed, risk scores and payments are expected to decrease, and the actual cost of care may not be fully reflected in the 2021 payments. Avalere also looked at telehealth utilization, as many MA plans are pivoting operations to this virtual form of administering care. In 2020, the Centers for Medicare & Medicaid Services (CMS) announced permanent changes to telehealth-related policies to respond to the virus, increasing flexibility and guidance. Without these swift moves, analysts indicate that utilization would have dropped more significantly than it already has. One of the changes CMS instituted allows telehealth claims to be submitted for risk adjustment if both audio and video are used to conduct the visit for inpatient, outpatient, or professional services.
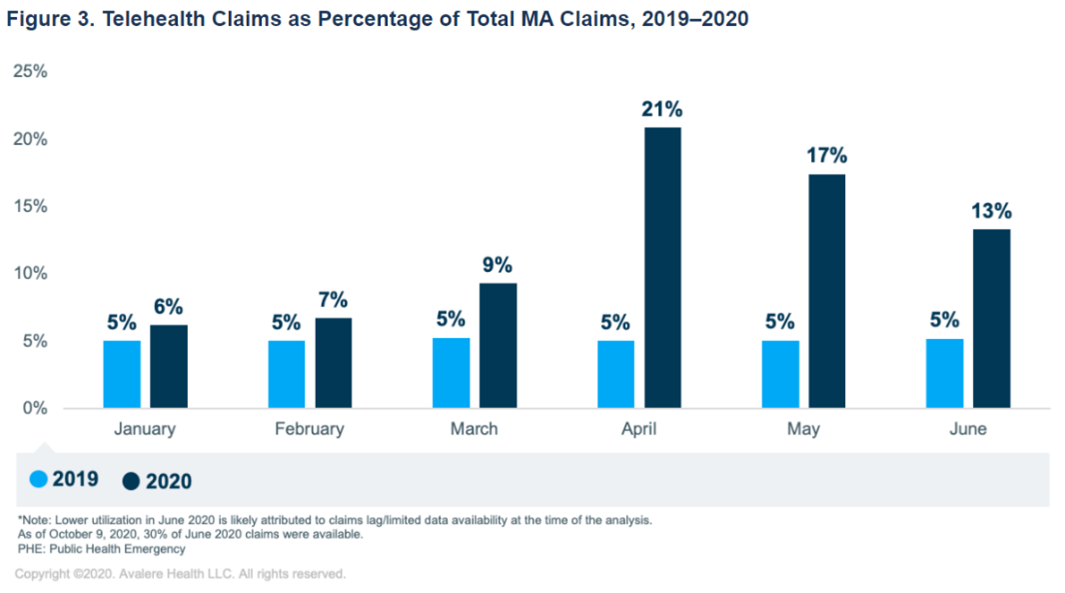
Fig. 3 displays the telehealth claims as a percentage of total MA claims between 2019 and 2020. From “COVID-19 Pandemic May Reduce MA Risk Scores and Payments.”
To predict the impact on risk-adjusted MA payments, analysts used the 2020 midyear score and the initial score for 2021. Focusing on the initial score for 2021, which factors in the first four months of the pandemic, the score revealed a 3.5% decrease in utilization and, consequently, a 2.39% decrease in payment. CMS will update 2021 risk scores this summer using the full year of 2020 data, which will include many COVID-19 months. Avalere modeled three scenarios based on assumed low, medium, and high utilization levels, leading them to predict that risk scores could decrease anywhere from 6.3 – 9.6% and potentially result in MA payments lowered as much as 6.1%.
Impacts to hierarchical condition category (HCC) capture based on the same 2020 and 2021 score data shows that 9% of all enrollees did not have any HCC codes recorded. Estimates for the percentage of enrollees without captured HCCs for the midyear 2021 adjustment are expected to increase in all three prediction models. Meanwhile, the comparison of enrollees with four or more HCCs recorded drops from about 31% to 22%.
Tried and True Risk Stratification Methods to Fill in the Gaps
As Medicare enrollees tend to be a vulnerable population, MA plans need to prepare for long-term effects post-pandemic. The community is often at the highest risk for COVID-19 due to the high occurrence of pre-existing conditions. Additionally, as revealed in utilization analyses, beneficiaries are likely not seeing their providers, perhaps due to fear of exposure, leading to worsening disease states. As the nation continues to navigate the PHE, MA plans will need to rely on new strategies, including telehealth, to offset the higher cost of care. They will also need to rely on tried-and-true methods of identifying high-risk patients, pushing for Medicare preventative appointments like annual wellness visits (AWVs), prioritizing coding and recapturing known HCCs with each encounter, and closing care gaps.
I want to invite you to join me on December 9, 2020, for Medicare Advantage: Staying Competitive in 2021 With CAHPS® Updates. In this webinar presentation, I will be discussing more key MA updates that will change in 2021, like the increase of the CAHPS® survey measures’ weight by four times, which will require providers to enhance training for their staff to improve the patient experience. I hope you can join but register anyway to receive a recording if you cannot.

Cindy Dyer is a Product Manager at Lightbeam.
